A Prescription for Change in Delaware
How health care providers can help curb the opioid epidemic.
Suspected Drug Overdose Deaths in 2025:
Data, provided by the Delaware Division of Forensic Science, are analyzed weekly from Friday to Thursday, and reported the following Friday. Last updated: 12/22/2025
Now Live: DTRN360 Provider Portal
Connecting providers across disciplines to track the progress of their behavioral health patients.
Prescription medications contribute to the opioid epidemic. You can change that.
Patterns of opioid prescribing, including dose, duration, quantity, co-prescribing, and patient risk factors, are major determinants of whether a person becomes dependent on or addicted to opioids. The prescribing of opioids for pain, as well as the abundance of these dangerous drugs in our medicine cabinets and communities, is significantly driving the opioid epidemic. According to the Substance Abuse and Mental Health Service Administration (SAMHSA), nearly 10 million Americans age 12 or older have misused pain reliever medication within the past year (National Survey of Drug Use and Health, 2018).
In 2017, Delaware issued new regulations for safer opioid prescribing and better pain management practices, supporting the CDC Guideline for Prescribing Opioids for Chronic Pain — United States, 2016 . The state’s Addiction Action Committee (AAC) guided the development of this page.
Sign up for updates and CME credit opportunities
Tools. Training. Teamwork.
Partner with us to reduce stigma and improve awareness and connection to treatment in Sussex County.
Learn MoreResources for:
Download or Order Materials
Order or print a variety of helpful, free materials in multiple formats and languages.
Access MaterialsDeaths due to opioid use continue to increase in Delaware.
In 2018, 400 individuals died from drug overdose, according to preliminary data from the Delaware Division of Forensic Science. Although illicit fentanyl usage has led to an increase in deaths, nearly 100 individuals died from non-fentanyl-related opioid prescriptions in 2017.
According to the National Institute on Drug Abuse, 80% of heroin users in the United States first misused prescription opioids. Also, the CDC estimates that 25% of individuals who use opioids to treat chronic pain develop an opioid use disorder (OUD).
Opioid-related overdose death rate per 100,000 people, 1999–2018 (age adjusted)
Percentage of drug overdose deaths by drug type, Delaware, 2017
Pie chart showing percentage of drug overdose deaths by drug type, Delaware, 2017CDC ranks Delaware first in the nation for high-dose and long-acting/extended-release opioid prescription rates.
Recent studies show that patients with high-dosage opioid prescriptions have much higher rates of opioid use disorder than do patients with low-dose prescriptions — across both short- and long-duration regimens.
Long-acting/extended-release opioid prescriptions are associated with greater risk of opioid use disorder.
Studies show that there are no clear differences in pain or function with long-acting/extended-release opioids, and more importantly, there is a greater risk of nonfatal overdose when starting treatment with long-acting/extended-release opioids (CDC, 2016).
Delaware continues to have the highest prescription rates for opioids over 90 MME and long-acting/extended-release opioids in the United States. The graphs below compare Delaware’s high-dose and long-acting/extended-release prescribing trends to those of the U.S., with Delaware’s rates consistently higher than the nation’s.
According to the CDC’s Annual Surveillance Report of Drug-Related Risks and Outcomes (2017) , opioid prescribing rates, including high-dose and long-acting/extended-release, continue to improve. It is critical that we remain steadfast in our focus on decreasing high-dose opioid usage and offer short-term opioid prescriptions. If opioids are used, prescribe the lowest effective dose.
Annual High-Dose (≥90 MME/Day) Opioid Prescribing Rates per 100 People
Annual Long-Acting/Extended-Release Opioid Prescribing Rates per 100 People
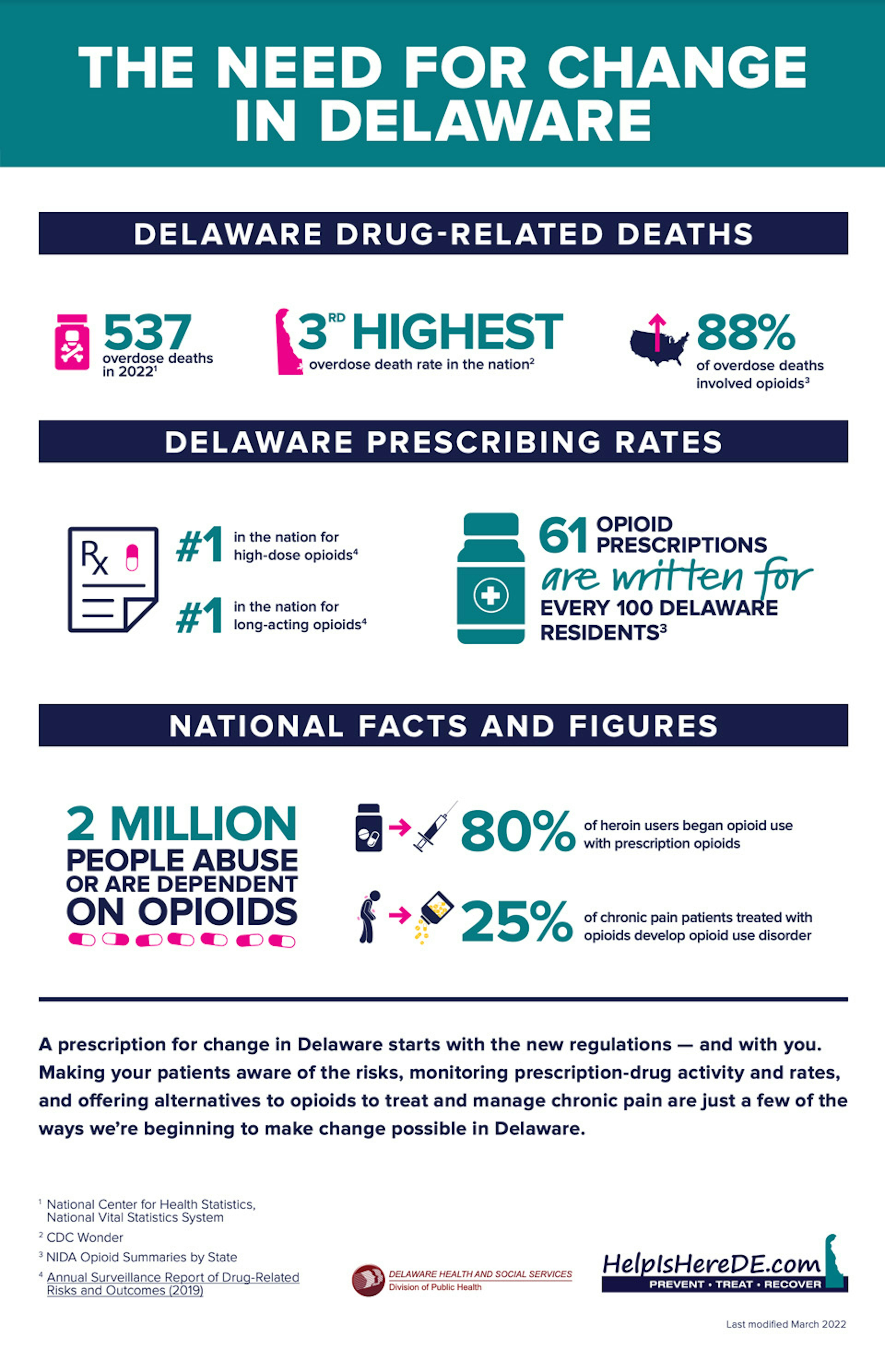
The Need for Change
A prescription for change in Delaware starts with the new regulations — and with you. Making your patients aware of the risks, monitoring prescription-drug activity and rates, and offering alternatives to opioids to treat and manage chronic pain are just a few of the ways we’re beginning to make change possible in Delaware.
(PDF, 217KB)