Educate Pregnant Patients About Substance Use
How to Educate Pregnant Patients About Substance Use
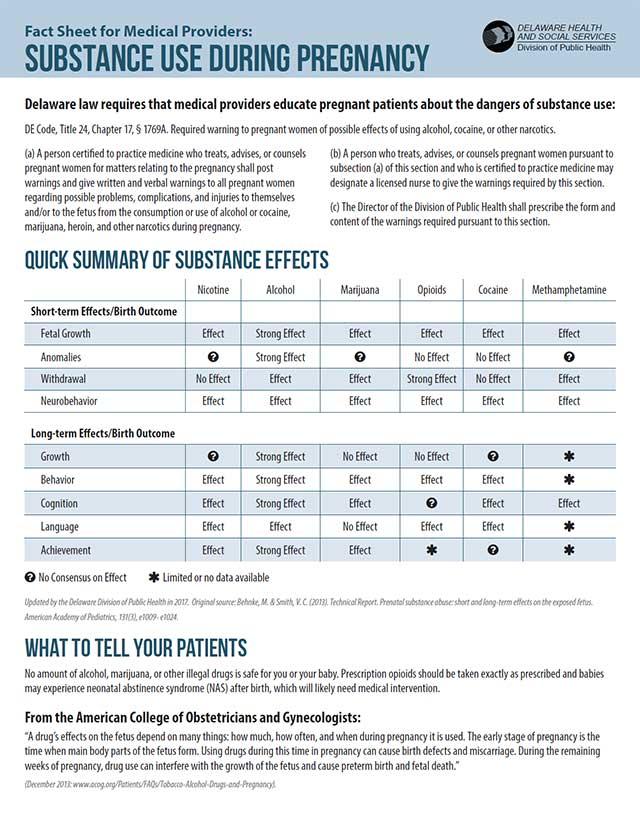
Delaware law requires medical providers to educate pregnant patients about the dangers of substance use:
DE Code, Title 24, Chapter 17, § 1769A. Required warning to pregnant women of possible effects of using alcohol, cocaine, or other narcotics.
- (a) A person certified to practice medicine who treats, advises, or counsels pregnant women for matters relating to the pregnancy shall post warnings and give written and verbal warnings to all pregnant women regarding possible problems, complications, and injuries to themselves and/or to the fetus from the consumption or use of alcohol or cocaine, marijuana, heroin, and other narcotics during pregnancy.
- (b) A person who treats, advises, or counsels pregnant women pursuant to subsection (a) of this section and who is certified to practice medicine may designate a licensed nurse to give the warnings required by this section.
- (c) The director of the Division of Public Health shall prescribe the form and content of the warnings required pursuant to this section.
What to Tell Your Patients
No amount of alcohol, marijuana, or other illegal drugs is safe for you or your baby. Prescription opioids should be taken exactly as prescribed, and babies may experience neonatal abstinence syndrome (NAS) after birth, which will likely need medical intervention.
From the American College of Obstetricians and Gynecologists (ACOG)
“A drug’s effects on the fetus depend on many things: how much, how often, and when during pregnancy [the drug] is used. The early stage of pregnancy is the time when main body parts of the fetus form. Using drugs during this time can cause birth defects or miscarriage. During the remaining weeks of pregnancy, drug use can interfere with the growth of the fetus and cause preterm birth or fetal death.”
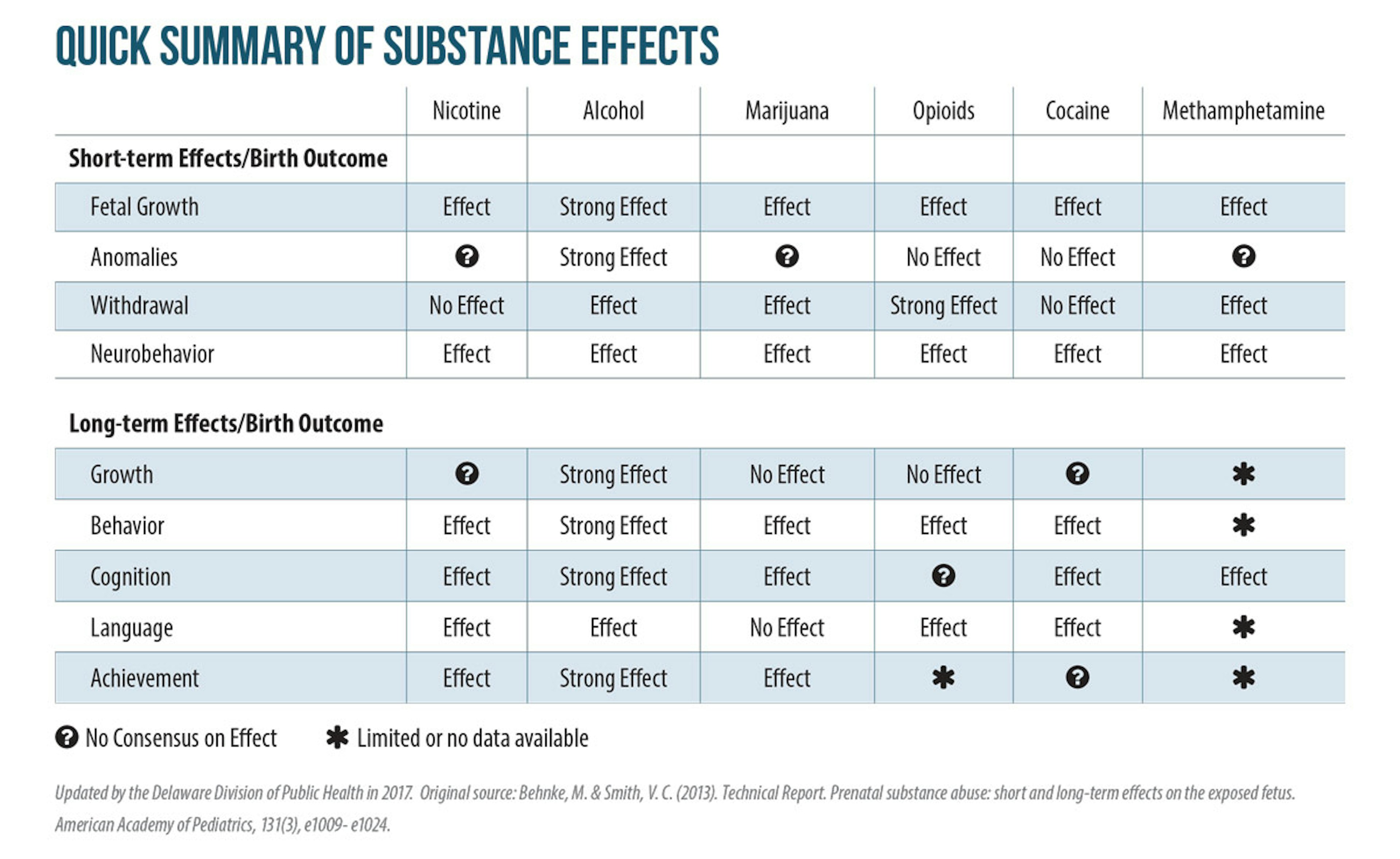
Alcohol
Alcohol is the primary cause of preventable birth defects. When a pregnant woman drinks alcohol, it reaches the baby through the placenta. While an adult’s liver will break down the alcohol, a baby’s liver cannot, and so the alcohol is significantly more toxic. Drinking alcohol during pregnancy can cause damage to a baby’s organs; physical, emotional, and behavioral problems as the child develops; difficulties in learning or memory; and higher incidence of attention deficit hyperactivity disorder (ADHD).
The damage caused by drinking alcohol is well documented and vastly underestimated.
Opioids: Legal and Illegal
Opioids are a highly addictive substance, and their use and abuse is driving the current addiction epidemic. Opioids can cause life-threatening withdrawal symptoms in babies, better known as neonatal abstinence syndrome (NAS). Symptoms include excessive crying, high-pitched cry, irritability, seizures, and gastrointestinal problems, among others. NAS requires hospitalization of the affected infant and possibly treatment with morphine or methadone to relieve symptoms. Treatment should also include nonpharmacological interventions, such as skin-to-skin contact and rooming in. Research on the long-term effects of opioid use during pregnancy is still evolving, but there is some evidence to suggest adverse behavioral and cognitive effects on children whose mother used opioids.
No patient should be counseled to immediately stop using opioids, including heroin. Suddenly stopping use could send the fetus into distress, threaten the pregnancy, and even cause miscarriage. Consistent with ACOG guidelines, physicians should discuss a broad range of treatment options, including medication-assisted treatment (MAT). For information on treatment programs or to learn more about MAT for pregnant women, call 833-9-HOPEDE.
Cocaine and Methamphetamine (Stimulants)
Pregnant women who use cocaine are at higher risk for maternal migraines and seizures, premature membrane rupture, and placental abruption (separation of the placental lining from the uterus). Cocaine could exacerbate cardiac problems — sometimes leading to high blood pressure (hypertensive crises), spontaneous miscarriage, preterm labor, or difficult delivery.
Babies born to mothers who use cocaine during pregnancy may also have low birth weights and smaller head circumferences, and may be shorter than babies born to mothers who do not use cocaine. These newborns also show symptoms of irritability, hyperactivity, tremors, high-pitched cry, and excessive sucking at birth.
Marijuana
Marijuana use should not be viewed as a safe alternative to other drugs. Contrary to reports, marijuana can be addictive. ACOG and the American Academy of Pediatrics (AAP) state that marijuana cannot be used safely during pregnancy. There is research to suggest that using marijuana during pregnancy can cause impaired neurodevelopment in fetuses, as well as low birth weight and problems in behavior and cognition in childhood. While more research must be done, ACOG states that the adverse effects of smoking marijuana to mother and fetus are well documented.
Tobacco
While this information focuses on alcohol, illegal substances, and prescription drug abuse, the negative impact of tobacco use on birth outcomes is also well documented. If a patient indicates that she smokes, consider referrals to the Delaware Quitline for free cessation resources and tools — at QuitNow.net/Delaware or by calling 1-866-409-1858.
How to Screen Pregnant Patients for Substance Use Disorder and Alcohol Use
ACOG recommends universal screening with brief intervention and treatment referrals for cannabinoids, alcohol, club drugs, dissociative drugs, hallucinogens, opioids, stimulants, tobacco, and other compounds such as anabolic steroids and inhalants.
You have an important role in educating women about the dangers of substance abuse during pregnancy, screening women for substance use disorder, and referring those with a potential substance use disorder. The goal is to help the mother and her baby.
Any pregnant woman who is on opioids — legal or illegal — should not cease her use immediately, because there could be significant risks to the fetus. Conversion to MAT is preferred for women seeking to discontinue use of illegal or legal opioids during pregnancy.
To learn more about MAT treatment locations for pregnant women, visit the Substance Abuse and Mental Health Services Administration (SAMHSA) website at samhsa.gov , or call 833-9-HOPEDE.
Pregnant women cannot be penalized under the law for substance use during pregnancy. Medical providers do not have a legal requirement or obligation to report substance use in pregnant women or to perform testing to confirm suspected use. In fact, it is outside of child protective services’ legal authority to take a report of a mother’s behavior while she is pregnant.
General Screening Recommendations
Step One: Start the Conversation
Following the Screening, Brief Intervention, and Referral to Treatment (SBIRT) model, start the conversation in a reassuring and compassionate manner. For example, you could say, “Can I ask you about drug or alcohol use? This information is important in working with you to have a healthy pregnancy.” Be reassuring. Be clear that the information will not be used against the patient or impact her ability to keep custody of the child. Emphasize the importance of your commitment to help her have a healthy pregnancy.
Step Two: Do the Screening
Use the screening tool that works best for your practice and your population. The next page includes three validated screening tools that can be used easily in a health care setting. All seek to identify potential issues that would require further dialogue with the patient and referrals to treatment providers for continued assessment. These screening tools are in the public domain and are recognized by SAMHSA.
General Screening Tools
“Screening” means using a validated screening tool to ask questions aimed at understanding the patient’s potential substance use. There are several validated screening tools for pregnant women, including 4 P’s and T-ACE, as well as CRAFFT for adolescents and young adults.
The 4 P’s (for substance abuse):
Scoring: Any “yes” should be used to trigger further discussion about drug or alcohol use. Any woman who answers “yes” to two or more questions should be referred for further assessment.
Source: Adapted from Ewing H Medical Director, Born Free Project, Contra Costa County, 111 Allen Street, Martinez, CA. Phone: 510-646-1165.
The T-ACE (for alcohol abuse):
Scoring: Any woman who answers the first question with “Three or more drinks” receives two points. Each “yes” to the additional three questions scores one point. A score of two or more is considered a positive screen, and the woman should be referred for further assessment.
Source: Sokol RJ, Martier SS, Ager JW. 1989. The T-ACE questions: Practical prenatal detection of risk drinking, American Journal of Obstetrics and Gynecology 160 (4).
CRAFFT — Substance Abuse Screening for Adolescents and Young Adults:
Scoring: Two or more positive items indicate the need for further assessment.
Source: Center for Adolescent Substance Abuse Research, Children’s Hospital of Boston. The CRAFFT screening interview. Boston (MA) CeASAR; 2009.
Step Three: Educate the Patient and Provide Referrals
If the screening tool does not identify a potential problem:
State law requires all medical providers serving pregnant women to counsel them on the dangers of alcohol, marijuana, and other drug use during pregnancy. Recommend that they cease use of all drugs, except opioids, which require special considerations and may need to involve MAT.
If the screening tool does identify a risk for substance use disorder:
Medication-Assisted Treatment (MAT)
MAT is an important part of the treatment plan for pregnant women and has shown improved outcomes. According to ACOG, “The rationale for medication-assisted treatment during pregnancy is to prevent complications from illicit opioid use and narcotic withdrawal; encourage prenatal care and drug treatment; reduce criminal activity; and avoid risks to the patient associated with a drug culture.”
The two main medications involved in MAT for pregnant women are methadone and buprenorphine (without Narcan). The decision regarding the most appropriate medication should be made jointly with the MAT provider, the obstetrician, and the woman.
Remind patients not to use alcohol or illegal drugs during pregnancy, and take to prescription medications exactly as prescribed.
Most people know that using illegal drugs, including marijuana and heroin, is not safe for the fetus during pregnancy, but many do not know that alcohol could be, or even more dangerous. Remind your patients that drinking alcohol and using illegal drugs while pregnant harms their baby, and that prescription drugs should be taken exactly as prescribed.
General Screening Tools and Recommendations
The American College of Obstetricians and Gynecologists (ACOG) recommends universal screening for alcohol and opioids, and that providers ask pregnant women about their marijuana use. If they are using, you should urge them to stop because of the risk of permanent damage to the baby.
There are several validated screening tools for pregnant women, including DAST and MAST (Kemper 1993), and CRAFFT (Chang 2011) for pregnant adolescents. Another tool to consider is 4P’s Plus (Chasnoff 1999).
Alcohol Dangers and Screening Tools
Alcohol is the leading cause of preventable birth defects in this country. Drinking alcohol during pregnancy greatly increases the chances that the fetus will develop a fetal alcohol spectrum disorder (FASD). According to the Centers for Disease Control and Prevention (CDC), up to one in every 20 schoolchildren FASD.
Signs and symptoms of the various FASDs range from mild to severe, and include a combination of physical, emotional, behavioral, and learning problems. Prenatal alcohol exposure is a frequent cause of structural or functional effects on the brain, heart, bones and spine, kidneys, vision, and hearing. It’s also associated with a higher incidence of attention deficit hyperactivity disorder (ADHD) and specific learning disabilities, such as difficulties with mathematics and language, information processing, memory, and problem-solving.
The American College of Obstetricians and Gynecologists (ACOG) recommends the T-ACE screening tool, specifically developed for use with pregnant women.
Ask patients four questions:
Any drinking during pregnancy requires education and intervention. Inform patients that any alcohol during pregnancy can harm their fetus, and offer resources to address drinking.
Additional Resources
Dangers of Substance Use During Pregnancy
Screening Pregnant Patients
Alcohol Use in Pregnancy
Brochure: Alcohol Use in Pregnancy
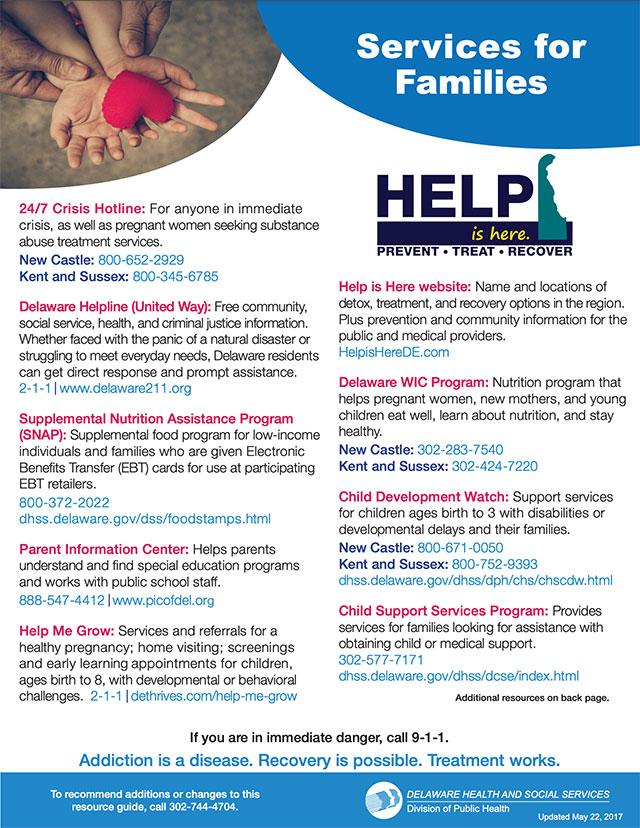
Services for Families
For additional health care provider resources on fetal alcohol and counseling patients, visit CDC.gov .
For additional OB-GYN-specific marketing materials, visit DEThrives.com .