Safe Prescribing Reduces Risk and Can Improve Outcomes
Improving the Way Opioids Are Prescribed Benefits Everyone
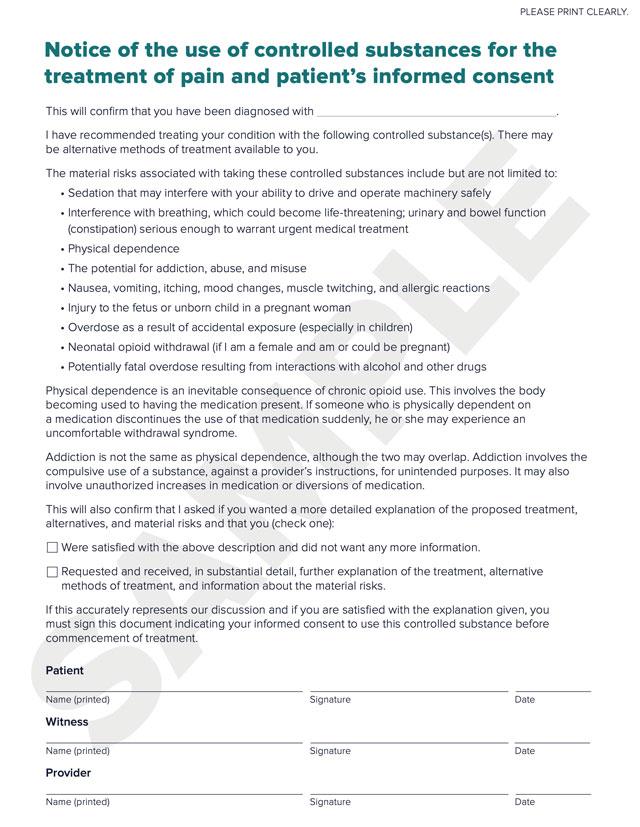
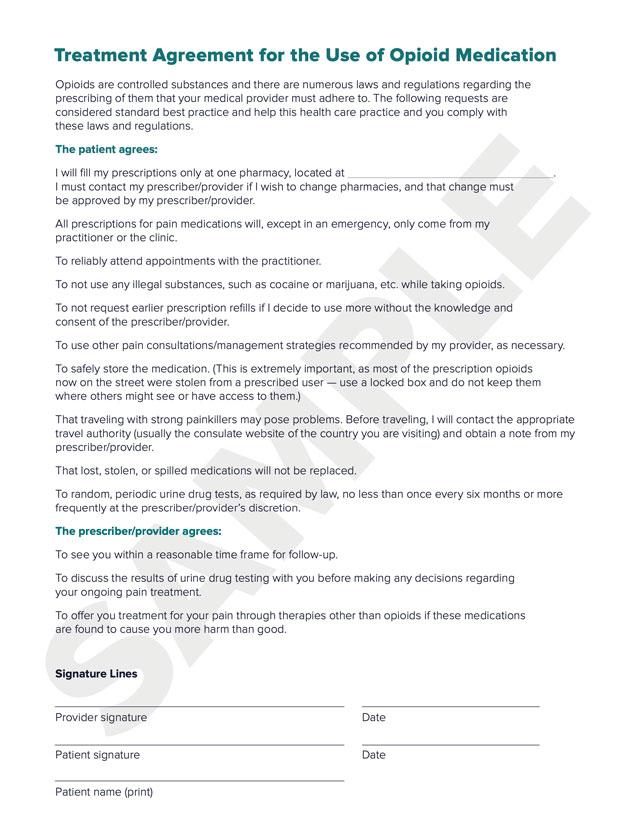
As a prescriber of controlled substances, you have both a professional responsibility and a legal obligation to abide by certain requirements in Delaware. Checking the Prescription Monitoring Program (PMP) before you issue certain prescriptions is mandatory. You also must participate in the two-part Controlled Substance Regulations (CSR) webinar upon receiving your first CSR license. Every two years after that, in order to renew your license to prescribe controlled substances, you must again complete the CSR webinar. CME credits are offered for webinar completion. You are also required to document informed consent and treatment agreements between you and your patients. These requirements not only help to keep your patients informed but can also help to reduce the threat of opioid-related overdoses and deaths in our state.
Sign up for updates and CME credit opportunitiesGuidelines for Prescribing Opioids Establish a Clear Decision-Making Process
The Centers for Disease Control and Prevention (CDC) has established specific guidelines for safely prescribing opioids, which include the following key recommendations:
- Opioids are not the first-line or routine therapy for chronic pain.
- Establish and measure goals for pain and function.
- Discuss benefits, risks, and availability of non-opioid therapies with patient.
- Use immediate-release opioids when starting.
- Start low and go slow.
- When opioids are needed for acute pain, prescribe no more than what’s needed.
- Do not prescribe ER/LA opioids for acute pain.
- Follow up and re-evaluate risk of harm; reduce dose or taper and discontinue if needed.
- Evaluate risk factors for opioid-related harms.
- Check PMP for high dosages and prescriptions from other providers.
- Use urine drug testing to identify prescribed substances and undisclosed use.
- Avoid concurrent benzodiazepine and opioid prescribing.
- Arrange treatment for opioid use disorder if needed.

Delaware Prescription Opioids Guidelines for Health Care Providers
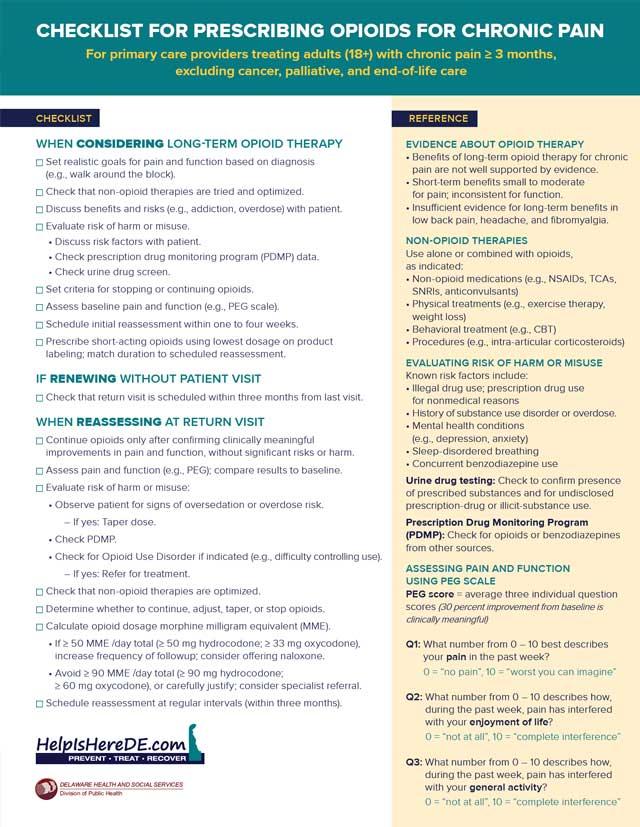
Refer to the CDC’s guide for prescribers to understand when opioids should be considered; what to do before starting opioid treatment for chronic pain; how to select opioid dosage, duration, follow-up, and discontinuation; and how to assess risks and harms.
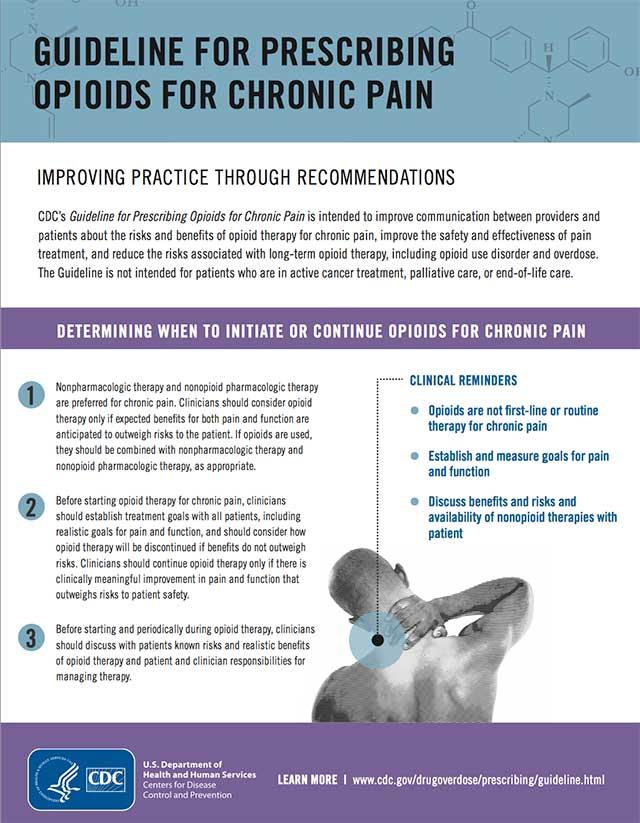
CDC Guidelines for Prescribing Opioids for Chronic Pain
Evaluate the benefits and harms with patients before initiating — and during — opioid therapy. Benefits and harms should be evaluated every three months, or more frequently.
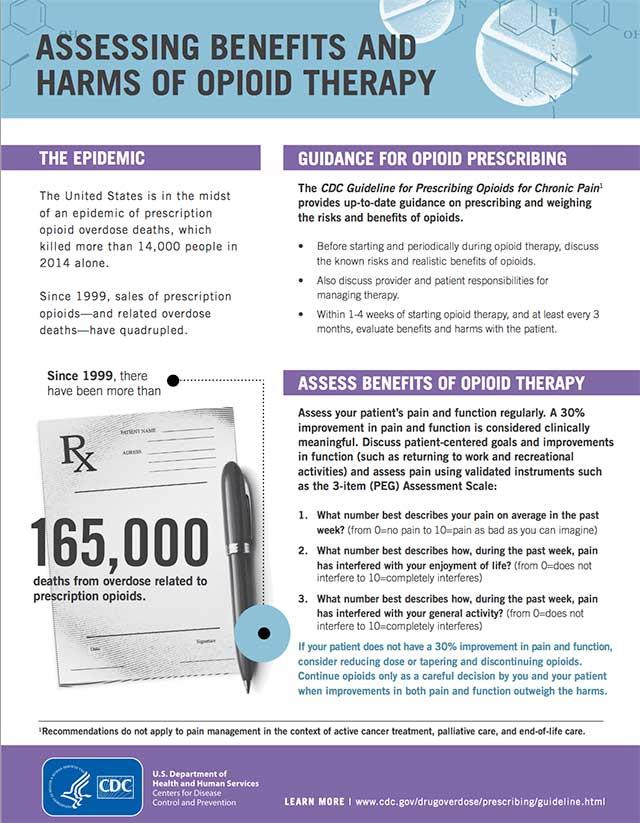
Assessing Benefits and Harms of Opioid Therapy
Use Proven Tools to Assess Pain and Risk
There are many ways pain affects your patients’ lives. The Pain, Enjoyment, and General Activity (PEG) evaluation can give you a simple, basic measurement of what they’re dealing with to help you determine the best therapy. But how can you determine if a patient could be a risk candidate in the future? Here are additional tools to help you use quantifiable measures to help determine the patient’s risk for substance abuse and addiction.
Assess your patients’ pain and function using the three-question PEG scale. Evaluating the level of pain and interference with the enjoyment of life and general activity on a scale of zero to 10 helps clarify the need for opioid therapy for chronic pain.
PEG Pain and Function Tool
Alternative Therapies Can Be as Effective as Opioids for Pain Management
Patients with pain should receive treatment that provides the greatest benefit. Opioids are not the first-line choice of therapy for chronic pain outside of active cancer treatment, palliative care, and end-of-life care. Evidence suggests that non-opioid treatments, including non-opioid medications and nonpharmacological therapies, can provide relief to those suffering from chronic pain, and are safer. Effective approaches to chronic pain include non-opioid medications and nonpharmacological treatments.
- Opioids should not be the first line of treatment for chronic pain.
- Non-opioid medications can be effective for treatment of chronic pain.
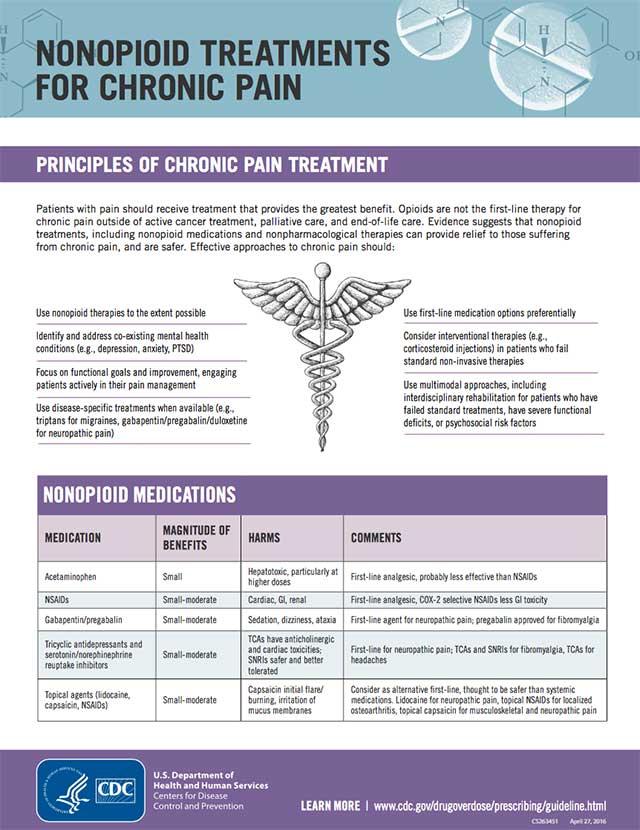
Non-opioid Treatments for Chronic Pain
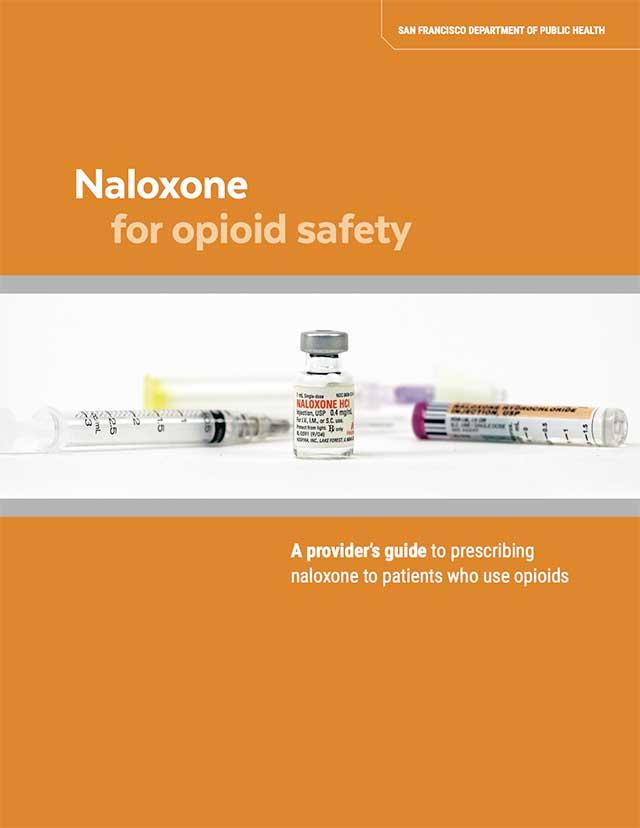
Naloxone Can Benefit Your Patients Who Are Prescribed High-Risk Medications
Naloxone can prevent an opioid overdose death by blocking receptor sites and reversing the toxic effects of the overdose. Prescribers should consider incorporating strategies to mitigate risk for overdose, including offering naloxone to all patients who are prescribed opioids. Use the concept of “risky medicines,” instead of “risky patients,” to frame your discussions and engage in proactive dialogue to minimize poisoning, oversedation, and overdose risk with patients who need opioid medications to improve function. Discussing an emergency overdose/poisoning/oversedation plan and possibly prescribing naloxone is an essential component of that dialogue.
Naloxone:
- Is a highly specific, high-affinity opioid antagonist used to reverse the effects of opioids.
- Can be safely administered by the average person via intramuscular or intranasal routes with virtually, no side effects and no effect in the absence of opioids.
- The effects last 30 to 90 minutes — usually sufficient for short-acting opioids, but emergency assistance should always be sought.
- While high doses of intravenous naloxone by paramedics have been associated with withdrawal symptoms, lower lay-administered doses produce much milder effects.
According to the CDC, the AMA Task Force to Reduce Opioid Abuse, and other authorities, patients considered at risk for opioid overdose are those who:
- Have a history of overdose or sedation
- Have a history of alcohol abuse or a substance use disorder
- Engage in active illicit drug use
- Are taking high daily doses of opioids (≥50 MME/day)
- Switch from one opioid to another
- Take opioids for pain and have respiratory problems
- Take opioids for pain and have renal/liver disease or other conditions such as hepatic disease, cardiac illness, or HIV/AIDS
- Take opioids and smoke, and have COPD, emphysema, asthma, sleep apnea, respiratory infection, or other respiratory conditions
- Are concurrently taking opioids and benzodiazepines or other sedatives
- Are taking opioids and antidepressants
- Are taking opioids and have an underlying mental health condition
- Have a high-risk score per the PMP
Before prescribing naloxone, determine the patient’s overdose risk and obtain a patient history:
- Review medications
- Take a substance use history
- Check the PMP
Take an overdose history — ask your patients whether they have:
- Overdosed or had a bad reaction to taking opioid medications
- Witnessed an overdose
- Received training to prevent, recognize, or respond to an overdose
You may also consider prescribing naloxone for at-risk patients:
- Who may have difficulty accessing emergency medical services (distance, remoteness)
- When the patient or caregiver has requested it
Two naloxone formulations are available:
Intramuscular (IM) injection and Intranasal (IN) spray are each available in two different forms.
| Intranasal | Intranasal | Intranasal | Intramuscular | |
|---|---|---|---|---|
| Strength | Intranasal Naloxone* 1 mg / 1 mL | Intranasal Naloxone* (4 mg / 0.1 mL) | Intranasal Kloxxado (8 mg / 0.1 mL) | Intramuscular Naloxone (0.4 mg / 1 mL) |
| Quality | Intranasal Two 2 mL prefilled Luer-Jet™ Luer-Lock needleless syringe PLUS two mucosal atomizer devices (MAD-300) | Intranasal #1 two-pack | Intranasal #1 two-pack | Intramuscular Two single-use 1 mL vials |
| SIG for suspected opioid overdose | Intranasal Spray 1 mL (half the syringe) into each nostril. Repeat after two to three minutes if no or minimal response. | Intranasal Spray full dose into one nostril. Repeat into other nostril after two to three minutes if no or minimal response. | Intranasal Spray full dose into one nostril. Repeat into other nostril after two to three minutes if no or minimal response. | Intramuscular Inject 1 mL in shoulder or thigh. Repeat after two to three minutes if no or minimal response. |
| Refills | Intranasal Two | Intranasal Two | Intranasal Two | Intramuscular Two |
*Approved naloxone variation under the Delaware standing order.
Download TablePatient instructions and counseling:
- Instruct patients how to administer if nonresponsive from opioid use, as well as how to assemble the naloxone injection or spray so that it can be administered.
- Include family and caregivers in patient counseling or instruct the patient to train others.
Higher Dosages — and Co-Prescribing — Are Associated with Higher Risk
Understanding dosage thresholds reduces the risk of harm to the patient. Calculating dosage can be complicated. Converting to morphine milligram equivalents (MME) helps to identify which patients are at increased risk. For example, patients who take dosages at or above 50 MME per day have twice the risk of overdose than those who take less. Calculations of MME are automatically figured by the PMP, based on data reported (prescriptions filled at pharmacies).
Co-prescribing opioids with other medications, especially benzodiazepines, can significantly increase the risk of overdose. According to the National Institute on Drug Abuse , more than 30 percent of overdoses involving opioids also involve benzodiazepines. Combining opioids and benzodiazepines can be unsafe since both types of drug sedate users and suppress breathing — the cause of overdose fatality — in addition to impairing cognitive functions.
A Urine Drug Screening Can Establish and Monitor Patient Risk
Urine drug testing can identify drug use that is not reported by your patients. Have an open conversation with your patient about urine testing so that they understand what the test may show, and explain that this is to help protect them and keep them safe from harm.

Urine Drug Testing Fact Sheet
Tapering and Discontinuing Opioid Therapy Should Be the Ultimate Goal
There are specific circumstances when you should consider tapering or discontinuing a patient’s opioid therapy. Those circumstances usually involve patients who:
- Aren’t seeing any meaningful improvement
- Request a dosage reduction
- Are taking dosages of 50 MME per day or higher without benefit, or are combining opioids with benzodiazepines
- Are exhibiting signs of substance use disorder
- Have overdosed or had another adverse event
- Show warning signs of an overdose risk, such as slurred speech, sedation, or confusion
CDC Guide: Tapering Opioids for Chronic Pain
Safely Disposing of Unused Opioids Protects Us — and the Environment
Of people who abuse prescription pain relievers, 70 percent get them from friends and relatives. To avoid having unused drugs fall into the hands of people for whom they were not prescribed, refer to the following recommendations to dispose of unused drugs with care.
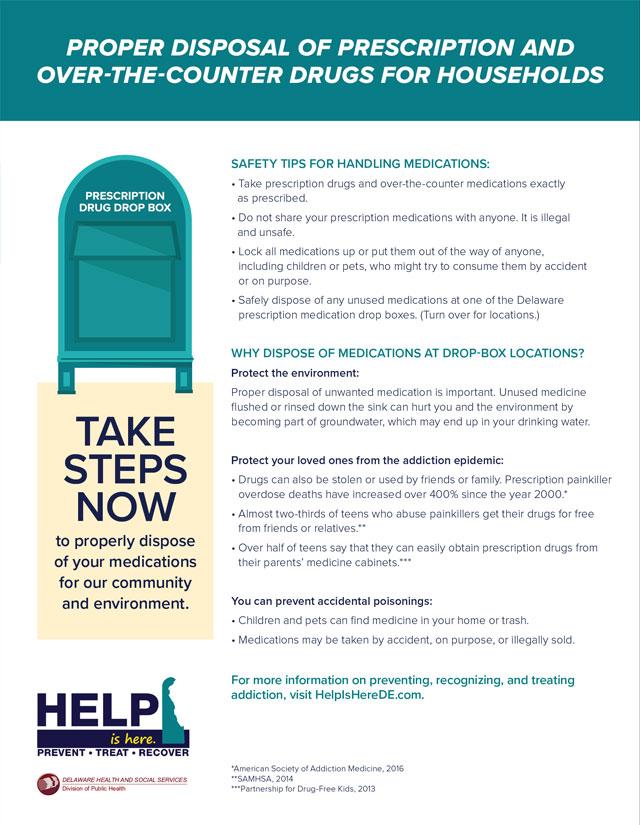
Prescription Drug Disposal
Educate Your Patients About Opioid Use and Risks
You may be considering opioids to help your patients manage chronic pain. Prescription opioids are often used to help relieve moderate to severe pain following a surgery or an injury, or for certain health conditions. These medications can be an important part of treatment, but they also come with serious risks. A fully informed patient is a better patient. Information can set expectations and make patients aware of the risks involved.
Prescription opioids carry serious risks for addiction and overdose, especially with prolonged use. An opioid overdose, often marked by slowed breathing, can cause sudden death. The use of prescription opioids can have a number of side effects as well, even when taken as directed:
- Tolerance, meaning you might need to take more of a medication for the same pain relief
- Physical dependence, meaning you have symptoms of withdrawal when a medication is stopped
- Increased sensitivity to pain
- Constipation
- Nausea, vomiting, and dry mouth
- Sleepiness and dizziness
- Confusion
- Depression
- Low levels of testosterone that can result in lower sex drive, energy, and strength
- Itching and sweating
Risks are greater with:
- History of drug misuse, substance use disorder, or overdose
- Mental health conditions (such as depression or anxiety)
- Sleep apnea
- Older age (65 or older)
- Pregnancy
Quick Facts:
- Drug overdose is the leading cause of accidental death in the United States.
- Opioid addiction is driving the drug epidemic.
- Opioids come with serious risk for addiction, abuse, and overdose.
Other pain management options may actually work better and have fewer risks and side effects:
- Acetaminophen (Tylenol®) or ibuprofen (Advil®)
- Cognitive behavioral therapy — a psychological, goal-directed approach in which patients learn how to modify physical, behavioral, and emotional triggers of pain and stress
- Exercise therapy, including physical therapy
- Medications for depression or seizures
- Interventional therapies (injections)
- Exercise and weight loss
- Other therapies such as acupuncture and massage